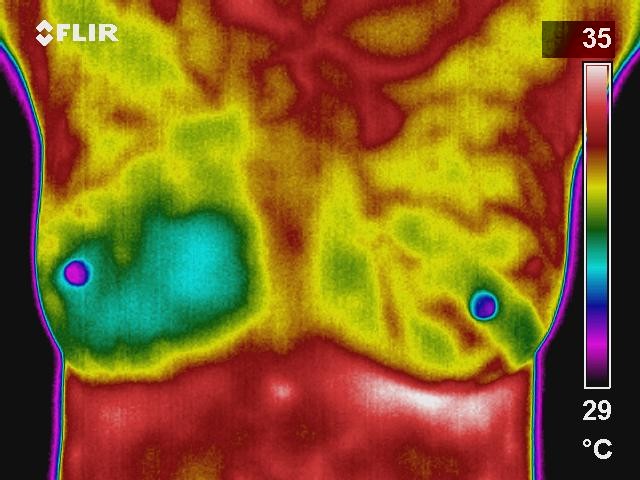
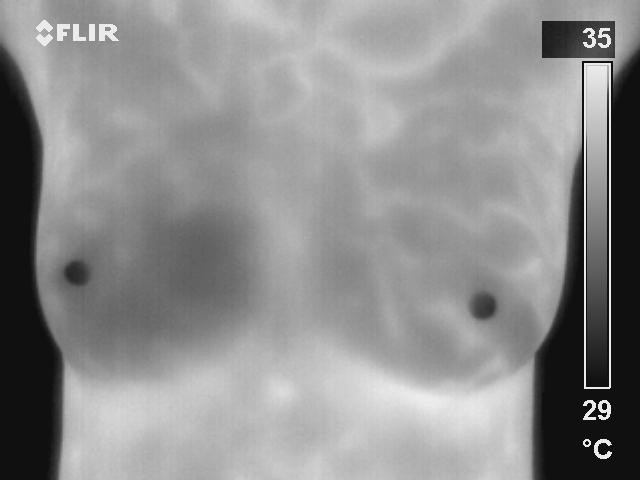
The use of Digital Infrared Imaging is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. In an ever-increasing need for nutrients, cancerous tumors increase circulation to their cells by holding open existing blood vessels, opening dormant vessels, and creating new ones (neoangiogenesis). This process frequently results in an increase in regional surface temperatures of the breast. We use ultra-sensitive medical infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution diagnostic images of these temperature variations.
Current methods used to detect breast cancer depend primarily on the combination of both physical examination and mammography. While this approach has become the mainstay of early breast cancer detection, mortality from this disease has gone relatively unchanged for 40 years. Since the absolute prevention of breast cancer has not become a reality as of yet, efforts must be directed at detecting breast cancer at its earliest stage. As such, the addition of Digital Infrared Imaging (Breast Thermography) may bring a great deal of good news for women.
WHAT MAKES DIGITAL INFRARED IMAGING SO UNIQUE:
Breast Thermography does not require radiation, compression, contact, or intravenous injection. As such, Breast Thermography is a very comfortable procedure which poses absolutely NO health risks to the patient.
Breast Thermography is based on detecting the increased blood vessel circulation and metabolic changes associated with a tumor’s genesis and growth.
Women who are on hormone replacement, nursing or have fibrocystic, large, dense, or enhanced breasts, etc... do not cause difficulties in reading Breast Thermography scans.
Just as unique as a fingerprint, each patient has a particular infrared map of their breasts. Any modification of this infrared map on serial imaging (images taken over months to years) can constitute an early sign of an abnormality. However, if cancer is suspected, this information is used to direct further examinations and tests. Breast Thermography’s ability to determine a woman’s future risk assessment, and its capability to frequently monitor this physiology with no health risks, is an important advancements in the field of breast imaging.
TECHNOLOGY, INTERPRETATION AND COMPARATIVE IMAGING
As is the case with mammography and all other imaging modalities, access to sophisticated technology and the expertise to interpret the findings are of prime importance. To help distinguish a normal process from an abnormal one requires proper training, clinical experience, strict adherance to protocols, and meticulous image acquisition. While not all tumors are visible on a mammogram, not all tumors are associated with a high level of blood vessel activity; thus, escaping infrared detection. Less aggressive lesions can be associated with less evident images. Therefore, in these select cases, Digital Infrared Imaging may become a prognostic indicator suggesting a much better overall prognosis.
When digitally produced, and interpreted by qualified doctors, abnormalities or changes in infrared images provide invaluable information. This is particularly true in patients with dense breasts, non-specific physical or mammographic findings, or women with a previous history of breast surgery or radiation. The use of serial infrared imaging can draw additional attention to areas that require further evaluation or closer scrutiny during initial or subsequent exams. This further evaluation may include additional imaging such as mammography, ultrasound, or MRI. Used as a complimentary imaging technique, recent data suggests that Digital Infrared Imaging may also help monitor the effects of some of the newer proposed anti-angiogenesis therapies (currently recognized as a promising treatment strategy).
EARLY DETECTION MEANS LIFE
Breast cancer is the most common cancer in women, and the risk increases with age. Risk is also higher in women whose close relatives have had the disease. Women without children, and those who have had their first child after age 30, also seem to be at higher risk. However, EVERY WOMAN is at risk of developing breast cancer. Current research indicates that 1 in every 8 women in the US will get breast cancer in their lifetime. In Trinidad it is said to have at least 1 new case every day.
Breast Thermography’s ability to detect signs of functional abnormalities, lies in its unique capability of monitoring the temperature variations produced by the earliest changes in tissue physiology (function). However, Breast Thermography does not have the ability to pinpoint the location of a tumor. Consequently, Digital Infrared Imaging’s role is in addition to mammography and physical examination, not in lieu of. Digital Infrared Imaging does not replace mammography and mammography does not replace Digital Infrared Imaging, the tests complement each other. Since it has been determined that 1 in 8 women will get breast cancer, we should use every means possible to detect abnormalities when there is the greatest chance for survival. Proper use of breast self-exams, physician exams, Digital Infrared Imaging, and mammography together may provide the earliest detection system available to date.